Pancreatic Disease, a vital organ nestled deep within the abdomen, plays a critical role in digestion and glucose regulation. However, when afflicted by disease, the pancreas can become a source of significant health complications and challenges. Exploring the intricacies of pancreatic disease sheds light on its causes, symptoms, diagnostic approaches, and treatment modalities, offering valuable insights into this complex medical condition.
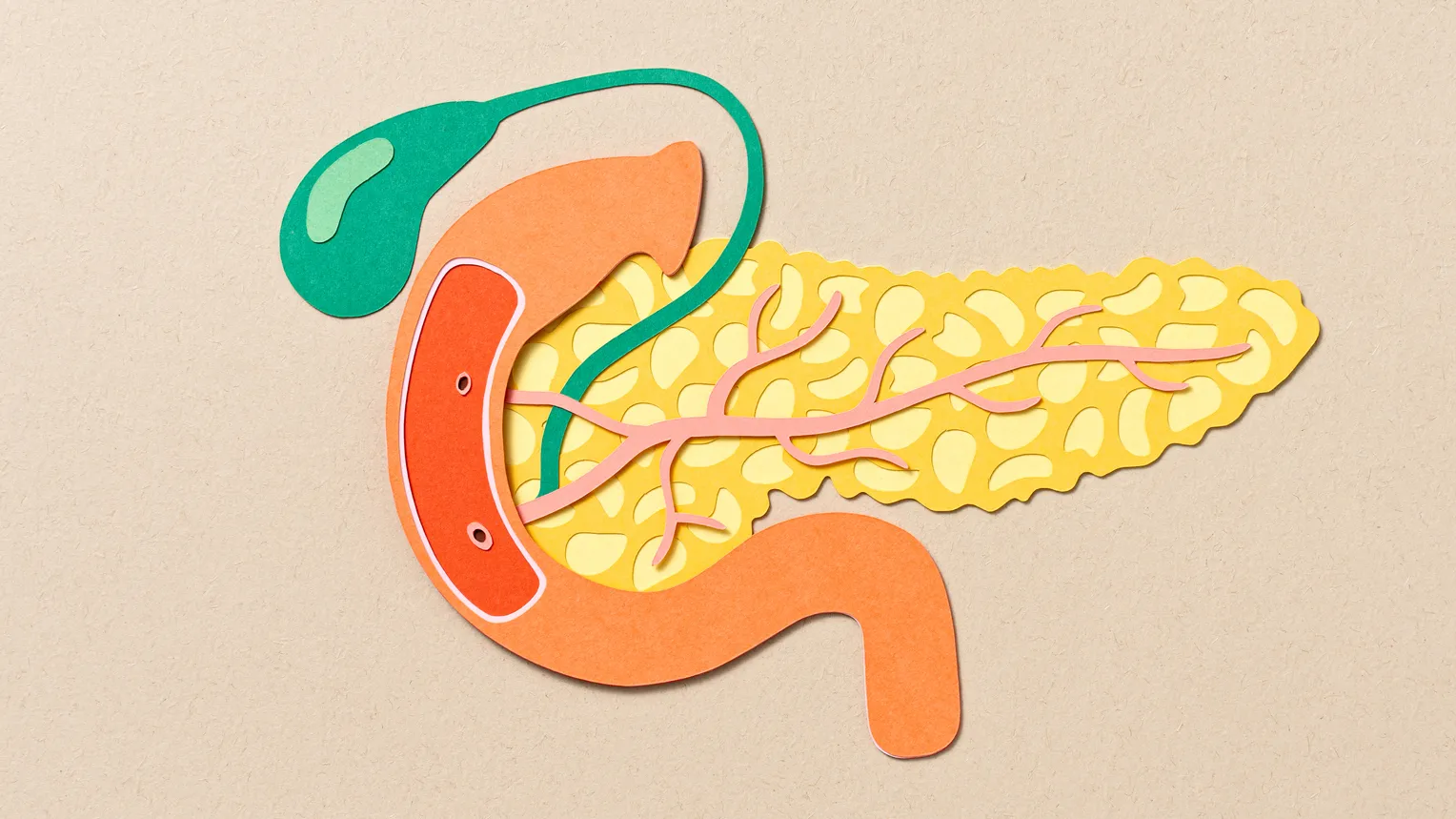
Anatomy and Function of the Pancreas
The pancreas, located behind the stomach, is a dual-function organ with endocrine and exocrine functions. Its exocrine component produces digestive enzymes that aid in the breakdown of fats, proteins, and carbohydrates in the small intestine. Meanwhile, the endocrine portion, consisting of clusters of cells called islets of Langerhans, secretes hormones such as insulin and glucagon, which regulate blood sugar levels.
Types and Causes of Pancreatic Disease
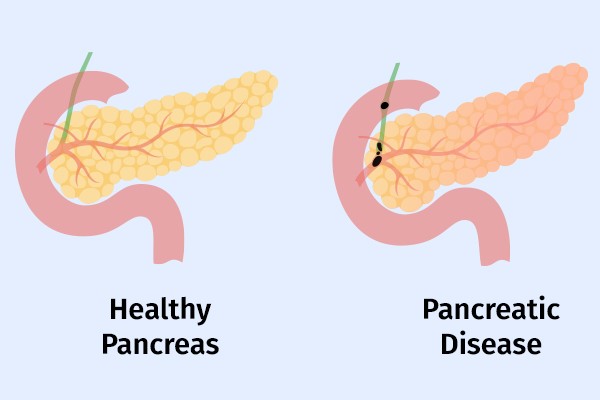
- Pancreatitis: Pancreatitis, characterized by inflammation of the pancreas, can be acute or chronic. Acute pancreatitis often arises from gallstones, excessive alcohol consumption, or certain medications, leading to sudden onset abdominal pain, nausea, and vomiting. Chronic pancreatitis, typically associated with long-term alcohol abuse or underlying conditions such as cystic fibrosis, manifests as persistent abdominal discomfort, weight loss, and malabsorption.
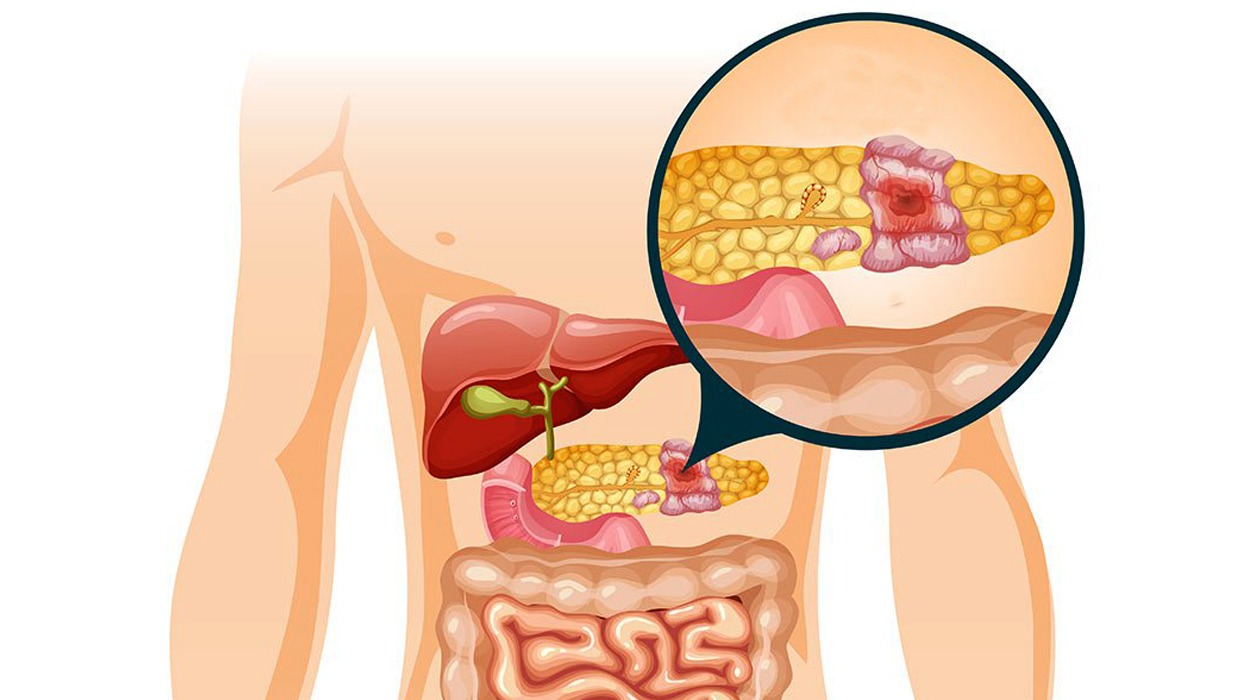
- Pancreatic Cancer: Pancreatic cancer, though relatively rare, is one of the deadliest forms of cancer, with a low survival rate. Most cases of pancreatic cancer originate in the cells lining the pancreatic ducts or the islets of Langerhans. Risk factors for pancreatic cancer include smoking, obesity, chronic pancreatitis, family history, and certain genetic mutations.
Symptoms and Diagnostic Evaluation
The symptoms of pancreatic disease vary depending on the specific condition and its severity. Common symptoms may include abdominal pain that radiates to the back, nausea, vomiting. Unexplained weight loss, jaundice (yellowing of the skin and eyes), and changes in bowel habits. Diagnostic evaluation typically involves a combination of imaging studies (e.g., ultrasound, CT scan, MRI), blood tests (e.g., amylase, lipase, tumor markers), and occasionally, invasive procedures such as endoscopic retrograde cholangiopancreatography (ERCP) or biopsy.
Treatment Approaches
The management of pancreatic disease depends on its underlying cause, severity, and stage of progression. Acute pancreatitis often requires hospitalization for supportive care, including pain management, intravenous fluids, and bowel rest. Chronic pancreatitis may necessitate lifestyle modifications (e.g., dietary changes, alcohol cessation). Pain management, enzyme replacement therapy, and, in severe cases, surgical intervention to alleviate obstruction or remove damaged pancreatic tissue.
For pancreatic cancer, treatment options may include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or a combination thereof. Early detection and intervention are critical for improving outcomes in pancreatic cancer. As the disease is often diagnosed at an advanced stage when treatment options are limited.
Pancreatic disease Represents a Multifaceted Medical Challenge
Encompassing a spectrum of conditions ranging from acute pancreatitis to pancreatic cancer. Despite advances in diagnosis and treatment, pancreatic disease remains associated with significant morbidity and mortality. Continued research efforts aimed at unraveling the underlying mechanisms. Identifying novel therapeutic targets, and improving early detection methods are essential for addressing the complexities of pancreatic disease and enhancing patient outcomes. Through interdisciplinary collaboration and comprehensive care, healthcare professionals strive to alleviate suffering, improve quality of life, and empower individuals affected by pancreatic disease to lead fulfilling lives.
The Lurking Danger: Assessing the Severity of Pancreatic Disease
Pancreatic disease, encompassing a spectrum of conditions from pancreatitis to pancreatic cancer, presents a formidable challenge to healthcare professionals and patients alike. Often dubbed the “silent killer,” pancreatic disease can evade detection until advanced stages, posing significant risks to health and survival. Understanding the gravity of pancreatic disease and its potential consequences is crucial for raising awareness, promoting early detection, and improving outcomes for those affected.
The Menace of Pancreatic Disease
Pancreatic disease carries a reputation for its insidious nature and dire prognosis. Whether in the form of acute pancreatitis, chronic pancreatitis, or pancreatic cancer.
The Perilous Path of Pancreatitis
Acute pancreatitis, characterized by sudden inflammation of the pancreas, can escalate rapidly, leading to severe complications such as pancreatic necrosis, infection, organ failure, and death. The underlying causes, which may include gallstones, alcohol abuse, or medication-induced injury, amplify the urgency of prompt diagnosis and intervention. Failure to recognize and treat acute pancreatitis in a timely manner can have devastating consequences, highlighting the gravity of this potentially lethal condition.
Chronic pancreatitis, marked by persistent inflammation and structural changes in the pancreas, imposes a relentless burden on affected individuals. The relentless cycle of pain, malnutrition, and pancreatic dysfunction diminishes quality of life and impairs daily functioning. Moreover, chronic pancreatitis can predispose individuals to complications such as pancreatic insufficiency, diabetes mellitus, pseudocysts, and even pancreatic cancer, compounding the long-term risks associated with this debilitating condition.
The Shadow of Pancreatic Cancer
Pancreatic cancer, notorious for its aggressive nature and dismal prognosis. Casts a dark shadow over the landscape of oncology. Often diagnosed at an advanced stage, pancreatic cancer offers limited treatment options and a grim prognosis. The insidious onset of symptoms, which may include abdominal pain, jaundice, weight loss, and digestive disturbances, underscores the challenge of detecting pancreatic cancer in its early stages when curative interventions are most effective.
The metastatic potential of pancreatic cancer, coupled with its resistance to traditional therapies. Amplifies the threat it poses to individual health and survival. Despite advances in surgical techniques, chemotherapy regimens, and targeted therapies, the overall survival rates for pancreatic cancer remain dishearteningly low. Highlighting the urgent need for continued research and innovation in the field of pancreatic oncology.
Conclusion: Confronting the Danger
Pancreatic disease, with its multifaceted manifestations and dire implications, demands our unwavering attention and commitment. From the acute onset of pancreatitis to the relentless progression of pancreatic cancer, the stakes are high, and the challenges are daunting. Yet, in the face of adversity, there is hope.
Through concerted efforts in research, education, early detection, and multidisciplinary care. We can confront the danger posed by pancreatic disease and strive towards improved outcomes and enhanced quality of life for those affected. By raising awareness, fostering collaboration, and advocating for resources and support. We can confront the lurking danger of pancreatic where its impact is minimized, and lives are saved.
Read More Article About “Meat Pie Delights: Exploring Global Variations and Flavors“

